Table of Contents
Healthcare BPO is a strategy enabling hospitals, clinics, care centers, and similar organizations to work with a third-party provider to lessen their administrative tasks and improve operational efficiency. Partnering with a trustworthy vendor helps them deliver high-quality patient care and service.
Medical billing outsourcing is a vital healthcare BPO service. This approach brings many benefits to healthcare organizations. However, submitting and managing claims or invoices for medical services rendered to patients is complex.
Keep reading to learn about the mechanics of medical billing outsourcing, its costs, and its benefits.
Medical billing outsourcing market: A quick glance
Grand View Research foresees a rosy future for the global medical billing outsourcing market, soaring to a hefty $30.2 billion by 2030. Until the forecast period, the industry will flourish at a compounded annual growth rate (CAGR) of around 12.26%—a promising sign for healthcare providers seeking operational enhancements and patients desiring seamless care.
The healthcare sector is experiencing increased clinical billing outsourcing. The uptrend is due to the obligatory installation of complicated International Classification of Diseases (ICD) 11 standards, growing healthcare expenses, and the federal duty to maintain electronic medical records (EMR) for reimbursement.
The report also notes that the COVID-19 pandemic accelerated the healthcare industry’s adoption of digital technologies. Amid challenges, medical providers have embraced digitalization and outsourcing to improve operations, leading to market growth and the development of digital healthcare infrastructure.
As the medical billing outsourcing market thrives, healthcare providers turn to business process outsourcing (BPO) companies specializing in revenue cycle management (RCM). This strategic shift, accelerated by the pandemic, underscores the industry’s pursuit of operational efficiency and a flawless patient experience.
How medical billing outsourcing works: The complete cycle
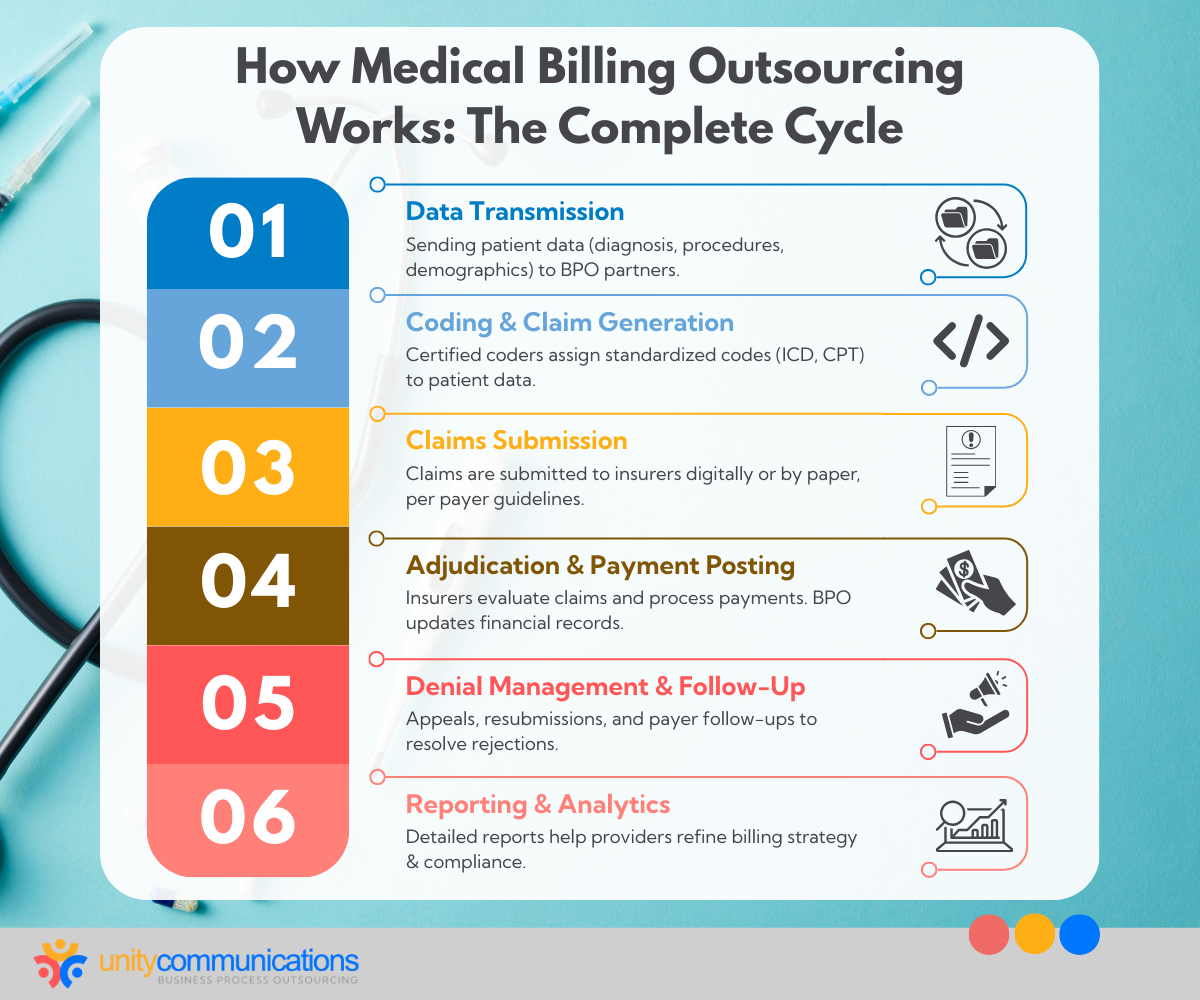
What is BPO in healthcare billing? It involves delegating medical billing tasks to a specialized service provider to increase efficiency, enhance patient services, and address associated concerns using industry best practices.
Medical billing outsourcing operations unfold in several interconnected stages, as discussed below.
Data transmission
A healthcare provider sends patient data, such as diagnoses, procedures, and demographic information, to medical billing outsourcing companies. The data is essential to generate medical claims.
Here are some data transmission challenges and how BPO providers address them:
- Diverse data formats. Medical billing includes various electronic health record (EHR) systems and management software that cause data format inconsistencies.
- Solution: BPO providers invest in robust data integration platforms to standardize data across different formats.
- Interoperable issues. Incompatibility between healthcare information technology (IT) systems prevents seamless data exchange.
- Solution: Service providers leverage interoperability standards such as Health Level Seven (HL7) and Electronic Data Interchange (EDI) for seamless communication between disparate systems.
- High data volume. Medical billing entails transmitting large quantities of data, straining communication channels.
- Solution: BPO organizations utilize high-bandwidth networks and scalable infrastructure to manage data.
- Lost/corrupted data. The disappearance of or damage to digitally stored information poses a significant challenge.
- Solution: BPO enterprises implement data recovery and error detection mechanisms to effectively prevent and address data integrity issues.
Coding and claim generation
Third-party professionals from a medical coding company meticulously assign medical codes to collected patient data per standardized systems, including ICD-11 and Current Procedural Terminology (CPT). The codes represent the services provided and guide claims generation.
Some data transmission issues and BPO solutions are outlined below:
Complex coding systems. Medical coding outsourcing involves navigating the ICD-10, ICD-11, and CPT systems, which require specialized knowledge and expertise. Solution: BPO providers employ certified coders with extensive training and experience to ensure accurate code assignments.
- Erroneous coding. Incorrect or incomplete coding can lead to claim denials or reimbursement delays.
- Solution: BPO companies implement quality assurance (QA) processes, including coding audits and peer reviews, to identify and rectify coding errors before submitting claims.
- Compliant coding practices. Keeping abreast of evolving coding regulations and guidelines is a crucial medical billing outsourcing function.
- Solution: Third-party vendors invest in ongoing training and education for their coding staff to ensure adherence to regulatory standards and minimize compliance risks.
Claims submission
Depending on each payer’s requirements, the onshore, nearshore, or offshore BPO firm transmits its generated claims to insurance payers online or on paper. This stage necessitates strict adherence to laws and attention to detail to reduce claim denials and delays.
Presented are some difficulties in claims submission, along with BPO providers’ strategies for resolution:
- Complex payer requirements. Insurance payers have diverse and intricate claim submission guidelines, leading to potential errors and rejections.
- Solution: Outsourcing providers stay updated on payer policies and utilize specialized software to ensure claims meet unique payer requirements.
- Inaccurate data. Incomplete patient and service information can result in claim denials or delays.
- Solution: BPO enterprises implement rigorous data validation checks and thorough documentation reviews to enhance claim accuracy before submission.
- Late submission. Prolonged claims submission can lead to payment delays and revenue loss.
- Solution: Third-party partners establish efficient workflows and utilize automated scheduling tools to ensure timely claim submission. They optimize the healthcare provider’s cash flow.
Adjudication and payment posting
Insurance companies assess claims upon receipt, evaluating their validity and calculating compensation amounts based on contract terms and coverage rules.
Depending on the agreement, payments are made to the healthcare provider or the medical billing outsourcing company once the case is resolved. Payment posting reconciles accepted payments with related claims and updates the provider’s financial records.
Highlighted are the obstacles to adjudication and payment posting and how BPO providers mitigate them:
- Rejected claims. Pinpointing denial causes, such as coding errors, can be a daunting medical billing outsourcing process for reimbursement maximization.
- Solution: BPO providers employ proactive denial management and corrective action plans to improve claims acceptance rates.
- Varied payments. Payment amounts vary based on contracts, deductibles, and copays. To maintain financial integrity, healthcare organizations must reconcile payments.
- Solution: BPO companies conduct detailed payment reconciliation for financial accuracy and compliance.
- Delayed payment posting. Challenges in processing and posting payments can disrupt cash flow and RCM for medical firms.
- Solution: BPO partners use real-time monitoring systems for timely intervention on payment discrepancies.
Denial management and follow-up
In cases of claim rejections or underpayments, the BPO business implements rigorous denial management measures with payers, such as appeals, resubmissions, and follow-up conversations. Timely resolution of rejections is critical to maximizing revenue and minimizing losses.
Enumerated below are the issues concerning denial management and follow-up and how BPO providers respond to them:
- Unknown root cause. Identifying denial causes, such as coding and eligibility issues, is tedious and requires thorough investigation.
- Solution: Third-party providers use analytics to determine denial trends, proactively reducing future denials.
- Slow or no follow-up. Prioritizing and managing follow-up tasks to ensure timely resolution, minimize payment delays, and prevent revenue loss can be an overwhelming medical billing outsourcing activity.
- Solution: To expedite claim resolution, BPO providers employ specialized teams with in-depth knowledge of payer policies, appeal procedures, and negotiation strategies.
- Unallocated resources. Proper resource distribution is required to balance workload demands, prioritize tasks, and optimize efficiency, maximizing revenue and cutting operating costs.
- Solution: BPO enterprises provide training to improve accuracy, documentation, and compliance, reducing denials due to avoidable errors or deficiencies.
Reporting and analytics
The healthcare offshoring services partner provides detailed reports and analytics, including claim acceptance and denial rates, empowering healthcare providers to refine strategies.
Uncover reporting and analytics challenges and how BPO firms tackle them:
- Strict compliance. Adhering to regulations, such as the Health Insurance Portability and Accountability Act of 1996 (HIPAA), while handling sensitive patient data might lead to legal and financial repercussions if overlooked.
- Solution: BPO firms follow strict security and compliance to protect patient data, including encryption, access controls, and audits.
- Complicated data QA. Implementing rigorous validation checks and similar quality control processes can be a formidable medical billing outsourcing task.
- Solution: BPO providers use comprehensive QA protocols (e.g., reconciliation processes and periodic audits) to identify and rectify data discrepancies to ensure the reliability of reporting outcomes.
- Inflexible solutions. Customizing reporting solutions to meet healthcare providers’ diverse needs and preferences can be intricate.
- Solution: BPO partners offer tailored reporting solutions with customizable dashboards and tools for medical providers to access and analyze billing data as needed.
Medical billing outsourcing costs: Understanding expense structures

Medical billing outsourcing fees or charges vary depending on the services provided, the healthcare organization’s requirements and operations, and the service provider’s BPO pricing model. Here are the costs and expense structures typically associated with this healthcare process.
Percentage of collections
Third-party vendors often charge a share of the total amount from successful insurance claims. These fees typically range from 4% to 6% of the managed funds. However, the price can shift based on the number of claims handled or the specific services offered.
Check the advantages of paying a percentage of collections:
- Aligned incentives. This model aligns the interests of the BPO company with the healthcare provider’s revenue goals. Since the outsourcing firm’s compensation is directly tied to the amount collected, team members are incentivized to maximize reimbursement and optimize RCM performance.
- Cost-efficient services. The structure offers cost-efficiency for healthcare providers with fluctuating billing volumes or variable reimbursement rates. Providers only pay the BPO firm a percentage of the revenue collected, eliminating fixed costs associated with in-house billing staff or flat fee arrangements.
Negotiating the percentage of collections involves minimum fees, exclusions, and metrics. Medical providers must ensure contract transparency to prevent billing disputes and misunderstandings.
Flat fee per claim
Alternatively, offshore outsourcing companies might charge a flat fee for each medical claim processed, regardless of the reimbursement amount. This medical billing outsourcing cost averages between $4 and $6 per claim, and it increases with more complex claims and BPO services.
Examine the positives of a flat fee per claim model:
- Predictable costs. Healthcare providers can predict outsourcing expenses accurately with a flat fee per claim, streamlining budgeting and financial planning.
- Simple to compute. Flat fees are straightforward, making them easy for the medical practice to understand and budget. They have no complex calculations or variable rates to consider.
- Suitable for low-volume practices. This model suits healthcare providers with lower claim volumes, avoiding overpayments for underutilized services by paying only for processed claims.
A flat fee could lead to higher costs for healthcare providers with multiple claims. Therefore, providers must assess whether this arrangement is an ideal pricing model for their practice beforehand.
Hybrid models
Some medical billing outsourcing companies offer hybrid pricing models, combining percentage-based and flat fees. For instance, a healthcare organization might pay a lower percentage of collections for claims with higher reimbursement amounts and a higher percentage for claims with lower reimbursement amounts.
Consider the merits of opting for hybrid models:
- Reduced risks. By diversifying the cost structure, hybrid models help mitigate risks associated with fluctuations in claim volumes, reimbursement rates, and payer policies. Healthcare providers can spread their financial risk across multiple pricing components.
- Better cost control. Hybrid models balance fixed and variable costs, offering better cost management benefits. Healthcare providers can profit from the predictability of flat fees while also taking advantage of the revenue-sharing incentives of percentage-based rates.
One downside of hybrid models is that they can be complex to manage due to their combination of different pricing components. Healthcare providers might find it challenging to understand and track the various cost elements, leading to confusion and administrative burden. As such, they must carefully assess hybrid model options for outsourcing.
Setup and onboarding fees
In addition to ongoing billing fees, healthcare providers might incur one-time setup and onboarding fees when collaborating with a medical billing outsourcing provider. These fees cover expenses associated with implementing billing software, training staff, and transitioning billing processes to the BPO partner.
While setup and onboarding fees are typically a one-time expense, they can significantly impact the initial cost of medical billing outsourcing, posing a barrier for smaller healthcare providers. These fees might increase the initial cost burden, straining budgets and cash flow.
Additionally, the time and resources required for onboarding might cause delays in adopting outsourced solutions, extending the transition period, and interrupting business. Mishandling the onboarding process results in inefficiencies and errors during the initial phases of outsourcing, impacting overall effectiveness.
Additional service fees
Depending on the scope of services offered, medical billing outsourcing companies might charge extra fees for value-added services such as credentialing, eligibility verification, coding audits, and reporting and analytics.
These fees are typically negotiated as part of the service contract or business process outsourcing agreement. They can differ due to the level of detail and recurrence of the additional services the healthcare practitioner requests.
Additional service fees in medical billing outsourcing can have drawbacks, including the potential for increased overall costs for healthcare providers, which can strain budgets, especially if multiple supplementary services are required.
Furthermore, the volatility of these fees makes it difficult for medical providers to precisely project expenditures, resulting in financial instability. The complexity of price structures and a lack of transparency might also lead to disagreements or misunderstandings between healthcare companies and outsourcing firms.
Penalties and chargebacks
Some agreements might include penalties or chargebacks for claim denials, rejections, or errors attributable to the outsourcing firm. These penalties are intended to incentivize the medical billing outsourcing provider to maintain high standards of accuracy and compliance in their processes.
Penalties and chargebacks in medical billing outsourcing can have significant drawbacks. Firstly, if not handled transparently or fairly, they can damage relationships between medical firms and BPO companies. Penalty disputes can strain partnerships and divert resources from patient care, affecting service quality.
The complex nature of penalty structures and the potential for subjective judgment in determining penalties can also introduce uncertainty and inconsistency into the billing process, further complicating matters for healthcare providers.
While penalties and chargebacks aim to incentivize accuracy, their drawbacks highlight the need for clear communication, fair practices, and effective resolution mechanisms in medical billing outsourcing partnerships.
Medical billing outsourcing benefits: Knowing and enjoying the perks

Outsourcing healthcare services offers pros and cons; healthcare providers must embrace these factors to optimize medical billing outsourcing and transform their operations. Consider the following benefits:
Enhanced efficiency to streamline processes
BPO providers handling healthcare billing responsibilities can improve productivity and effectiveness by achieving tasks faster and more accurately. These capabilities lead to streamlined processes and optimized outcomes.
Let us check the positive outcomes in detail:
- Improved patient experience. Higher efficiency contributes to a positive patient experience. Patients benefit from faster insurance reimbursements, reduced billing errors, and improved communication regarding their financial responsibilities. These perks enhance their overall satisfaction with healthcare services.
- Advanced technology integration. Medical billing outsourcing partners typically leverage advanced software and technology platforms to simplify billing processes. These include electronic claims submission, automated coding tools, and real-time claims tracking programs to boost efficiency and accuracy.
- Reduced administrative burden. Outsourcing medical billing tasks alleviates administrative burden on healthcare providers’ staff, allowing them to pay more attention to patient care. Thus, BPO increases productivity and efficiency within the healthcare organization.
Optimized RCM for better revenue
BPO companies leverage medical coding, claims processing, and denial management expertise to optimize RCM. This results in expedited claim reimbursement, reduced claim denials, and improved revenue realization for healthcare providers.
Discover the upsides of an efficient RCM:
- Improved cash flow. Optimized RCM ensures timely submission and processing of claims, resulting in faster reimbursement. Healthcare providers receive payments more quickly, improving cash flow and financial stability.
- Enhanced revenue capture. Efficient RCM maximizes revenue capture for healthcare providers. Proper coding, thorough documentation, and diligent follow-up on unpaid claims ensure that medical firms receive full reimbursement for services rendered.
- Financial stability. Optimized RCM ensures financial security for healthcare organizations. Improved cash flow, reduced billing errors, and enhanced reimbursement rates contribute to long-term financial health and sustainability.
Specialized expertise for accurate billing
BPO vendors employ seasoned professionals with specialized knowledge of medical billing regulations, payer policies, and coding intricacies. This expertise ensures compliance with industry standards and maximizes revenue capture through accurate coding and claims submission.
Uncover the perks of specialized expertise:
- Deep knowledge of billing regulations. Medical billing experts stay updated on evolving healthcare laws and payer requirements. They navigate complex billing regulations to ensure accurate claims submissions and compliance with billing standards.
- Accessible medical coding experts. BPO companies employ skilled professionals proficient in medical coding. Trained coders accurately assign codes to medical procedures and diagnoses. This process ensures compliance with coding guidelines for accurate billing, maximizing reimbursement.
- Improved adaptability to industry changes. BPO partners adapt quickly to changes in healthcare regulations and industry standards. Their specialized expertise allows them to implement new coding guidelines and billing practices seamlessly, ensuring continued compliance and revenue optimization.
Significant cost savings for budgeting success
Medical billing outsourcing enables healthcare providers to mitigate operating expenses associated with maintaining an in-house billing department. The predictable cost structure of outsourcing solutions facilitates financial planning and budgetary adherence.
Look into the favorable impacts of cost savings:
- Re-allocated funding. Outsourcing medical billing allows the excess funds from cost savings to be channeled to crucial areas, such as patient care, technology upgrades, staff training, and facility improvements. This enhances overall healthcare services and infrastructure.
- Budgetary adherence. Medical billing outsourcing helps organizations stick to planned spending limitations. This prevents overspending and enables healthcare providers to budget resources strategically. It fosters financial stability and supports long-term organizational growth and development.
- Enhanced financial performance. Cost savings achieved through outsourced medical billing contribute to better financial performance for healthcare providers. Reduced overhead and training costs lead to increased profitability and sustainability.
Increased focus on core competencies for first-rate patient service
One of the benefits of outsourcing in the healthcare industry is that medical companies can concentrate on their strong suits while leaving non-core functions, such as coding and billing, to specialized BPO providers.
Scrutinize the benefits of focusing on core competencies:
- Strategic growth opportunities. Transferring non-core activities such as medical billing frees internal staff for growth initiatives. Healthcare organizations can invest in expanding services, acquiring new technology, or entering new markets. They can drive long-term growth and success.
- Improved organizational focus. Zeroing in on core strengths sharpens organizational alignment. Offloading non-core tasks matches resources with strategic goals, boosting effectiveness and competitiveness.
- Elevated patient care. Outsourcing medical billing tasks lets healthcare providers prioritize patient care. They can enhance service quality and satisfaction through improved treatment and attention to patient well-being.
Scalable operations for consistent quality delivery
BPO companies specializing in medical billing outsourcing can adjust resources, staffing levels, and processes based on fluctuating workload demands. This flexibility allows healthcare providers to offer consistent service levels and optimize resource utilization.
Explore the boons of scalable processes:
- Sustainable growth. Scalable outsourcing solutions can adapt to healthcare providers’ growing needs. Outsourcing partners can scale operations to accommodate increased billing volumes and complexity as providers expand their practices or add new services.
- Quick response to market changes. Scalable activities enable healthcare providers to respond quickly to market or regulatory changes. BPO partners adjust operations for new requirements, reducing disruptions to RCM amid regulatory revisions.
- Consistent service levels. Scalable operations maintain quality service, even during peak periods, ensuring reliable revenue cycle management support.
The bottom line
Healthcare providers must find the ideal BPO partners to help them navigate the complexities and challenges of medical billing outsourcing. Third-party vendors have the assets, expertise, and connections to help organizations streamline billing processes, ensure compliance, and optimize revenue generation.
Before partnering with a service provider, healthcare firms must weigh the pros and cons of medical billing and coding. They must consider cost, efficiency, and the impact on overall RCM.
Let’s connect if you want to learn more about medical billing outsourcing and how we can tailor solutions for your unique needs!




