IN THIS ARTICLE
Table of Contents
Business process outsourcing (BPO) offers healthcare practices an efficient way to streamline operations and improve financial management. Small and midsized businesses (SMBs) leveraging BPO services for medical billing can optimize their revenue cycle and improve accuracy while reducing administrative overhead.
Partnering with a reliable BPO firm is key to maximizing these advantages. In this article, you will learn about the top medical billing outsourcing companies and the best practices for evaluating these firms to find the right BPO partner. Keep reading!
Criteria for selecting top medical billing outsourcing companies
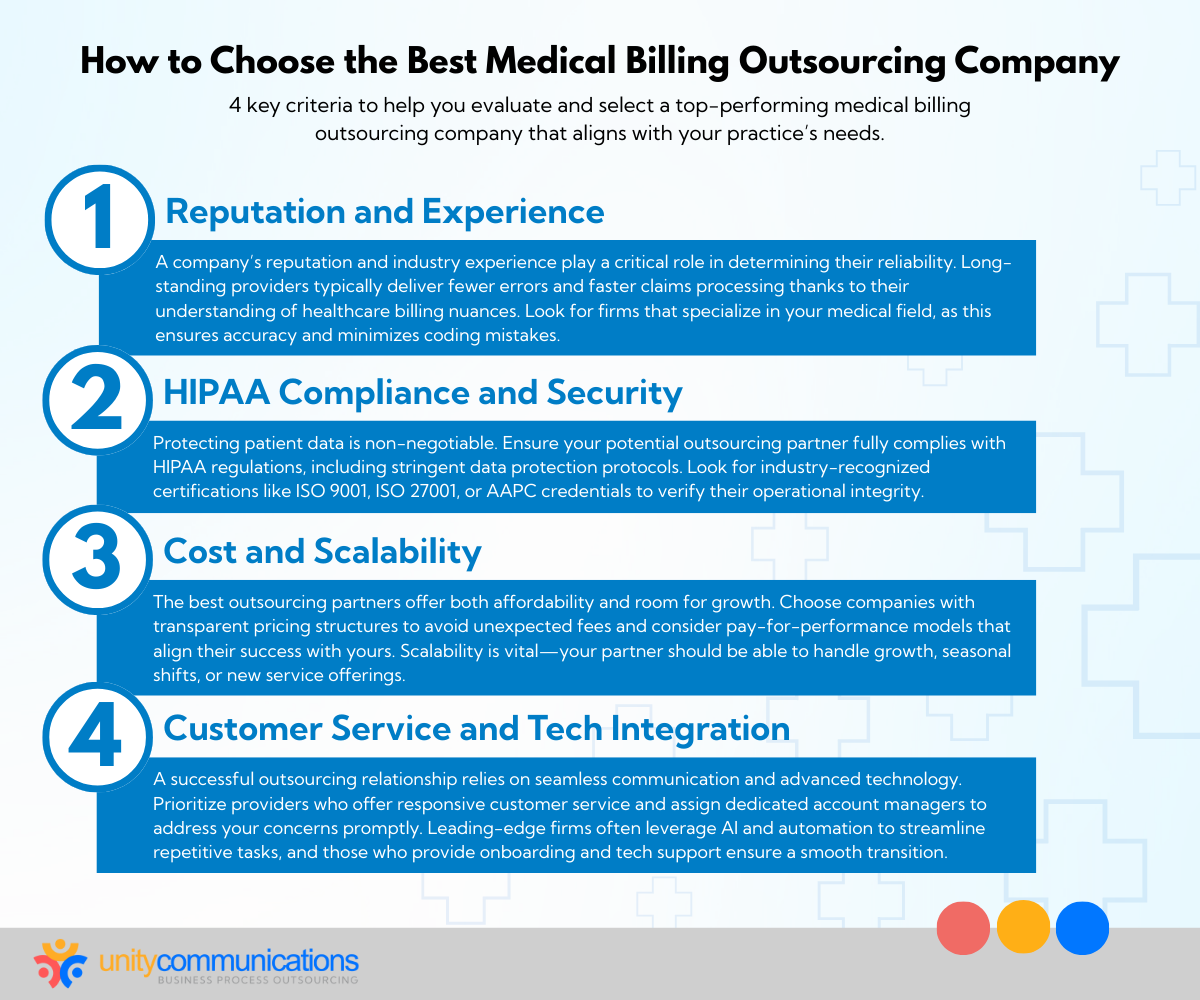
Outsourcing your medical billing operations begins by choosing a service provider. Understanding what to look for in BPO companies simplifies decision-making and connects your practice with a firm that fits your needs. Let’s explore the essential criteria to consider:
Reputation and experience
A solid reputation and proven track record are indispensable when evaluating potential BPO partners. Dependability, professionalism, and consistency drive a successful outsourcing initiative. Here’s how to research a medical billing outsourcing company with good standing and the necessary expertise:
- Years of industry experience. Companies with a lengthy history of healthcare billing outsourcing can face obstacles and adapt to industry trends. Their knowledge leads to fewer errors, faster claim processing, and more consistent results.
- Specialization in medical fields. Look for service providers specializing in your practice area, whether cardiology, pediatrics, or orthopedics. Field-specific expertise decreases coding errors and improves claim submission accuracy.
- Customer retention rate. Strong client loyalty demonstrates consumer happiness and consistent service quality. Seek testimonials, reviews, and case studies demonstrating long-term client connections.
- Performance metrics. Inquire about claim acceptance rates and turnaround times. A third-party provider with swift, efficient operations can help maximize your cash flow.
- Reputation in the healthcare community: Determine whether other medical professionals in your field endorse the BPO company. Recommendations might help strengthen their credibility and connection with your needs.
- Commitment to constant advancement. Choose a third-party vendor that keeps up with industry trends, regulatory changes, and technological improvements. This indicates that they are a forward-thinking partner for your practice.
HIPAA compliance
Compliance with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and relevant regulations is another criterion when short-listing top medical billing outsourcing companies. Verifying the BPO firm meets strict legal standards safeguards your practice’s reputation and patients’ trust. Take the pointers below:
- Conformity to HIPAA standards. The potential service provider must adhere to all protocols for protecting patient data. BPO and HIPAA compliance can help protect sensitive information and avoid penalties.
- Industry certificates. Check for ISO 9001 or 27001 and similar quality management certifications or organizational credentials, including the American Academy of Professional Coders (AAPC). These reflect the billing service company’s commitment to ethical and precise operations.
- Solid data security methods. Check their disaster recovery strategies and procedures against data breaches. These include encryption technology, safe server infrastructure, and frequent security audits.
- Access control policies. Determine whether the provider uses rigorous access controls, such as role-based permissions and multi-factor authentication, to prevent unauthorized access to critical patient information.
- Employee training programs. Confirm that the medical billing outsourcing companies frequently instruct their employees on HIPAA guidelines. Employees who have received proper training are less likely to violate regulations.
Cost and scalability
Top medical billing outsourcing companies offer cost efficiency and scalability, allowing businesses to maintain budgets while accelerating growth. Although affordability is ideal, the cheapest option might not be the best choice for your practice. Examine these factors instead:
- Transparent pricing structures. Ask for a detailed breakdown of expenses to avoid hidden fees. Understand what is included in their BPO pricing models, such as software, training, or follow-up claim services.
- Pay-for-performance models. Some third-party contractors offer pricing tied to their revenue, aligning their success with yours.
- Scalable solutions. A BPO partner that can grow with your practice means long-term viability. Ask how they handle fluctuating claims volumes or adapt to new services your practice might offer.
- Value over cost. Consider the benefits of outsourcing in the healthcare industry, such as reduced administrative workload. Factor in the potential time saved and how this strategy can let your team focus on patient care.
- Flexible contract terms. Look for service providers that offer adaptable options in their agreements, allowing you to adjust terms as your needs change without excessive penalties.
- Performance-based incentives: Some BPO companies offer bonuses or discounts based on their performance, which can align their motivation with your practice’s success, enabling mutual growth and cost savings.
Customer service and technology integration
Customer service and technology integration are pivotal to working smoothly with your outsourcing partner. The ideal collaborator emphasizes effortless communication between parties and uses technology to optimize billing workflow.
Your prospective medical billing outsourcing companies should have the following features:
- Responsive customer service. Choose an outsourcing firm that offers prompt and helpful support. It should also provide you with dedicated account managers and specialists to resolve issues quickly.
- User-friendly software solutions. The service provider’s billing software should integrate smoothly with your existing systems. Compatibility reduces manual entry errors and streamlines processes.
- Real-time updates and reporting. Look for helpful features, including live dashboards, regular reporting tools, and automated notifications for claim statuses. These provide clear visibility into claim statuses and billing performance.
- AI and automation. Outsourcing and artificial intelligence (AI) can enhance claim accuracy and speed. Automation reduces repetitive tasks, allowing you to focus on strategic areas of your practice.
- Training and support. Some BPO companies offer onboarding and training for your team to provide smooth technology adoption. Robust support systems keep disruptions to a minimum.
- Customizable solutions. Verify that outsourcing firms offer billing solutions tailored to your practice’s needs. These processes can enable workflow adaptability and improve efficiency without compromising quality.
Top medical billing outsourcing companies
BPO firms might specialize in different niches, offering tailored solutions to specific business requirements. The key is to find service providers that align with your needs and goals. Here are the leading medical billing outsourcing companies and their profiles to jumpstart your search.
Unity Communications

Unity Communications is a versatile outsourcing partner that provides a full range of services, including medical billing, call center operations, and customer support. The BPO company is well-known for its dedication to delivering first-rate customer service. It focuses on improving revenue cycle management (RCM) and optimizing billing operations for healthcare providers.
Strengths
- Comprehensive services: offers various services, from medical billing to claims management
- Experienced team: handles complex billing and coding, maintaining accuracy
- Cost-efficiency: caters for small and medium practices, balancing cost with quality
- HIPAA compliance: adheres to HIPAA standards to secure patient data handling
- 24/7 support: provides round-the-clock assistance for billing and claims issues
Specializations
- Medical billing efficiency: enhances claim acceptance rates and reduces errors using advanced technology
- RCM: specializes in improving cash flow and cutting administrative costs
- Multichannel support: focuses on excellent customer service through call centers, chat, and email
- Tailored solutions: delivers customized billing solutions for specialties, including pediatrics and cardiology
GeBBS Healthcare Solutions

GeBBS Healthcare Solutions is a technology-enabled RCM service provider dedicated to enhancing healthcare providers’ billing processes. Its advanced technology and comprehensive solutions make it a suitable outsourcing partner in the healthcare sector.
Strengths
- Expertise in RCM: has extensive experience managing and optimizing the entire revenue cycle
- AI-enabled technology: uses the latest AI tools to improve claims management and streamline billing operations
- Compliance focus: commits to maintaining high standards of compliance, which is critical in healthcare
- Proven track record: successfully partners with over 300 healthcare organizations, demonstrating reliability and effectiveness
- Customer-centric approach: emphasizes first-rate customer service with dedicated support and responsiveness
Specializations
- Comprehensive RCM services: provides end-to-end RCM solutions for various healthcare settings
- Risk adjustment solutions: focuses on risk adjustment coding and HEDIS initiatives
- Patient contact solutions: addresses patient eligibility, authorization, and follow-up
- Extended business office services: tackles compliance issues and claim rejections
- Coding and compliance auditing: maintains coding accuracy and compliance auditing for financial health
Apex EDI (Ensora Clearinghouse)
Apex EDI is a prominent electronic data exchange (EDI) solution provider for healthcare businesses. Its unique technologies and dedication to customer service make it an indispensable partner for optimizing billing operations and increasing revenue cycles.
Strengths
- Competence in EDI solutions: possesses extensive experience with electronic claims processing and management
- User-friendly technology: provides easy-to-use digital tools that make billing more manageable and efficient
- Dedicated support crew: has prompt customer service to help patients and consumers with their requirements and questions
- Budget solutions: concentrates on cost-effective programs that assist healthcare providers in getting reimbursed faster
- Commitment to conformity: maintains compliance with industry norms and laws, reducing errors in claim processing
Specializations
- Electronic claims submission: allows for rapid submission of claims to payers
- Payment posting services: simplifies payment reconciliation for healthcare providers
- Reporting and analysis: provides information on claims performance and financial health
- Integration capabilities: supports integration with a variety of practice management systems to improve functionality
R1 RCM
R1 RCM is a top outsourcing provider of technology-driven RCM solutions dedicated to transforming healthcare providers’ revenue cycles. Their innovative services boost operational efficiency and financial performance, strengthening the revenue cycle of its healthcare clients.
Strengths
- Experience with RCM: has expertise in managing and optimizing the revenue cycle for healthcare enterprises
- Operational efficiency: implements procedures to streamline operations, lower costs, and increase collection rates
- Patient-centered strategy: focuses on improving the patient experience, which leads to higher satisfaction and engagement
- Data-driven information: uses analytics to gain insights for decision-making and enhance financial outcomes
- Established performance record: has effective agreements with a diverse range of healthcare providers, demonstrating reliability
Specializations
- End-to-end RCM services: provides solutions that address all parts of the revenue cycle
- Patient access solutions: improves patient eligibility verification and appointment scheduling
- Claims management: streamlines claims processing to eliminate denials and speed up payouts
- Financial performance enhancement: grows net patient revenue (NPR) and overall financial health
eCatalyst Healthcare Solutions
Now part of e4health, eCatalyst Healthcare Solutions is a medical billing outsourcing company offering health information management (HIM) and coding solutions. Its commitment to quality and compliance highlights its focus on supporting clients with accurate coding, efficient claims management, and optimized revenue cycles.
Strengths
- Proficiency in HIM: has Extensive experience in health information management, including coding and auditing services
- Quality assurance: concentrates on sustaining high data accuracy and clinical documentation integrity standards
- Tailored solutions: delivers customized services that address the specific needs of various healthcare facilities
- Proven accomplishment history: has successfully worked with many hospitals and healthcare systems across the United States, showing reliability and effectiveness
- Dedicated support: supplies responsive customer service with emphasis on client satisfaction
Specializations
- Clinical documentation improvement (CDI): refines documentation practices to retain compliance and accuracy
- Auditing services: conducts extensive reviews to sharpen coding accuracy and compliance
- Health information technology (IT) consulting: offers skills in optimizing health computer systems for better performance
Omega Healthcare Management Services
Omega Healthcare Management Services is an RCM solutions provider for medical firms, payers, and pharmaceutical companies. With expertise in streamlining revenue cycles and maintaining compliance, Omega stands out for its tailored approach and advanced technology integration.
Strengths
- RCM expertise: offers end-to-end solutions covering patient access, mid-cycle services, business office functions, and clinical enablement
- Technology-driven processes: uses AI, machine learning (ML), and robotic process automation for coding, billing, and claim management, reducing errors and optimizing efficiency
- Global talent pool: employs over 7,000 skilled coding specialists across onshore and offshore locations for service scalability
- Education and retention: trains coders through Omega Medical Coding Academy and offers certifications, enhancing staff proficiencies
- Industry thought leadership: provides ongoing education and webinars for healthcare professionals
Specializations
- Medical coding and auditing: has expertise in reducing compliance risks and improving accuracy
- Claims management: enhances claim-to-cash cycles through automated tools
- Physician practice RCM: tailors solutions for specialties, including radiology, cardiology, and anesthesiology
PracticeAdmin
PracticeAdmin offers innovative practice management and billing solutions designed for medical practices and billing professionals. Its streamlined, cloud-based systems enhance efficiency and profitability, making it a trusted partner for healthcare providers.
Strengths
- Comprehensive platform: has a complete solution integrating billing, scheduling, and receivables management for seamless operations
- User-friendly design: offers intuitive platform developed by billing experts to reduce learning curves and enhance productivity
- Automation features: provides advanced tools for claims error detection and payment processing to streamline workflow
- Cloud-based technology: secures data management without hardware requirements, providing easy access from anywhere
- Flexible pricing: has pay-as-you-go models, including support, upgrades, and clearinghouse fees for cost transparency
Specializations
- Customizable scheduling: offers solutions for multi-facility, multi-provider setups with automated reminders and flexible calendars to reduce no-shows and optimize bookings
- Efficient billing: invests in streamlined tools for claim submission, error correction, re-submissions, and automated reporting, improving payments and financial outcomes
- Analytics and reporting: provides 100+ reports offering insights into patient flow, revenue trends, and operational efficiency
How to assess top medical billing outsourcing companies
These top companies can help SMBs navigate the pros and cons of medical billing and coding outsourcing, which can feel overwhelming for those venturing for the first time. However, asking the right questions and evaluating compatibility are necessary to find the right partner.
Here are the best practices for assessing a vendor for outsourced billing and collections:
Questions to ask during the consultation
Well-structured questions during initial consultations help establish a strong collaboration foundation and assess whether a third-party partner aligns with your practice’s needs. These inquiries enable you to evaluate the effectiveness and reliability of a healthcare BPO provider, confirming its ability to handle complex billing tasks effectively.
- What is your experience with practices of our size and specialty? Understanding whether the company has handled medical billing for similar healthcare settings helps assess its ability to manage your requirements.
- How do you handle claim rejections and denials? Ask about their error correction and claim resubmission processes. A robust system improves cash flow, showcasing the BPO impact on small businesses by minimizing errors and optimizing financial operations.
- What technology do you use for billing and reporting? Evaluate if the medical billing outsourcing companies use advanced software, such as AI tools, to streamline operations and improve billing accuracy.
- How do you maintain compliance with HIPAA and other regulations? Compliance with data security and privacy standards is non-negotiable in healthcare. You must understand how the company protects sensitive patient information.
- Can you provide examples of your past successes? Ask for case studies or client references to gain insight into their past performance, especially regarding reducing claim rejection rates and optimizing RCM.
- How do you handle patient inquiries and follow-ups? Inquire about their system for managing patient interactions, such as billing inquiries. Effective communication improves patient retention and satisfaction.
- What is your process for handling sensitive data? Inquire about encryption methods and data protection measures to secure patient information. A solid commitment to BPO security and HIPAA compliance is vital to minimize risks.
Evaluating compatibility with your needs
Aside from the questions, assessing the medical billing outsourcing companies’ suitability with your specific requirements is critical to finding a long-term partner. Here are vital points to consider when evaluating a vendor’s capacity to integrate into your practice’s workflow:
- Flexibility and customization. Each practice has unique billing processes based on specialties, patient demographics, and claim types. Look for a BPO firm offering customized solutions to your needs, including integrating practice management software and providing personalized workflow for outsourcing medical bills.
- Services scalability. If your practice plans to grow or expand, check if the third-party contractor can scale its services. Whether adding new specialties, increasing patient volume, or opening additional locations, your outsourcing partner should adapt to meet changing demands.
- Customer service and support. Effective communication, proactive issue resolution, and responsive account managers are essential. Consider whether the company offers 24/7 support. This is crucial when leveraging BPO for small businesses, helping maintain efficiency and smooth billing processes in your practice.
- Cost and pricing models. Although cost shouldn’t be the only factor, SMB healthcare firms must assess each potential partner’s pricing model. Whether pay-per-service, flat fees, or tiered pricing, verify the pricing is transparent and aligns with your budget and billing volume.
- Performance metrics. Look for medical billing outsourcing companies providing quantifiable or measurable results. Ask about acceptable and clean claim rates, average payment turnaround times, and denial management efficiency. Strong performance in these areas can improve your practice’s cash flow.
- Technology integration. Evaluate whether the service provider’s technology includes electronic claim submissions, automated patient statements, real-time payment tracking, and seamless integration with existing systems.
The bottom line

Finding the right partner from the leading medical billing outsourcing companies is critical for enhancing your practice’s efficiency and financial performance. Thorough research and due diligence can help you choose a service provider that meets your needs.
Ready to elevate your billing processes? Let’s connect and explore how partnering with a reliable service provider such as Unity Communications can improve your operations and cash flow. Contact us today to start optimizing your practice’s billing system!





