Written by Rene Mallari
Contents
The Covid-19 pandemic has been a game-changer in the global business landscape. Healthcare claims are one of the hardest-hit processes, so the insurance industry is still reeling from the effects.
As a result, policyholders’ requests for payments from their insurers have gone through the roof. Many carriers turned to business process outsourcing (BPO) to manage the rising number of claims.
Outsourcing to healthcare BPO providers help insurers overcome their challenges.
This article details the pandemic’s impact on medical claims and how outsourcing can help the industry. Keep reading to learn more.
The Pandemic’s Impact on the U.S. Healthcare Claims Industry

An S&P Global study estimated that U.S insurance carriers would spend about $90 billion in healthcare claims due to the pandemic. This would result in losses that might push them to use their reserves to cover the expenses. The medical costs of the global health crisis could hit $30 billion in the best-case scenario.
It added that approximately 50 million insured people, or close to 30% of the insured million, would contract the virus. This group is covered under Medicare, Medicaid, personal health insurance plans, and the small employee category. In a severe outbreak, outpatient claims for doctor visits and testing might reach nearly $13 billion.
The study notes that costs could be around $18 billion for a moderate outbreak, similar to a severe flu season, while a severe pandemic could drive hospital costs to $80 billion. Such spending would force insurers to take between 90% to 97% of revenue from the premium collection for medical claims reimbursements. The number of patients requiring hospitalization would hit 8 million across the country.
The financial strain would still be significant for affected insured individuals. The report forecasted they would still pay roughly $3.5 billion out of pocket for treatment after a moderate outbreak. During a severe outbreak, out-of-pocket costs would go as high as $16 billion.
The Pandemic’s Impact on Healthcare Claims Costs and Premium Rates
Simon Dreyer, vice president, and chief actuary for Global Health at Reinsurance Group of America (RGA), explains the factors affecting healthcare claims costs. He also discusses the challenges these factors present in determining future premium rates.
Dreyer says that in terms of claims costs, the pandemic led to increased hospitalization expenses to treat infected patients. But this was partly offset by decreased healthcare demand during lockdowns when health systems put off or canceled non-emergency care due to increased capacity and public fear.
He also cites other factors that might impact claims costs, such as:
- Vaccinations and testing
- Psychological effects of the pandemic
- Overall health impairment for patients with past severe infection
- Expenses on extra personal protective equipment (PPE)
Dreyer adds that the pandemic made it challenging to predict future insurance premiums for two reasons:
- The long-term effect of the pandemic on claims costs remains unknown.
- Past healthcare claims experience before the outbreak in 2020 has become unreliable for pricing purposes.
He points out that insurance providers have much to consider regarding the deferred care and higher-than-expected claims that occurred in 2020 and 2021 respectively. Analyzing these trends is vital in resolving the premium rating issue.
The Pandemic’s Impact on Healthcare Claims: Remote Work Issues
The pandemic forced many employees in the insurance sector to adopt a work-from-home (WFH) policy. Since then, remote work has become an obstacle in-house claims departments.
Managing insurance claims entails a high volume of paperwork and large amounts of data. Working in a new environment while dealing with the surge in medical claims leads to processing inefficiencies and errors.
Additionally, claims adjusters find it difficult to do their jobs properly under a WFH arrangement. These insurance professionals estimate the amount to pay claimants, so they rely on physical availability. In particular, high-value or complicated claims are harder to resolve without a physical inspection of the location for insurance investigation.
The Pandemic’s Impact on Healthcare Claims: Data Security Issues
According to Digit Insurance, healthcare claims jumped almost four times in 2021 compared to 2020. The significant rise is due to the public’s increased awareness of health insurance products after the pandemic. But the upsurge in claims made cybersecurity, compliance, and fraud a more serious concern.
The primary challenge for insurers is handling and protecting the ever-growing volumes of claims against cyberattacks and data breaches.
Insurance carriers process numerous sensitive patient and insurance records daily. They might suffer huge financial losses and reputational damage if such records fall into the wrong hands.
With prominent data breaches becoming increasingly common, government laws and industry standards will be updated more frequently. Insurers will find it tougher to comply with those rules and standards now than before because they have a lot on their plates.
This is where outsourcing comes in. BPO companies can help carriers manage healthcare claims and other processes to address the challenges brought about by the pandemic and other factors.
10 Ways Outsourcing Can Aid Healthcare Claims Processing
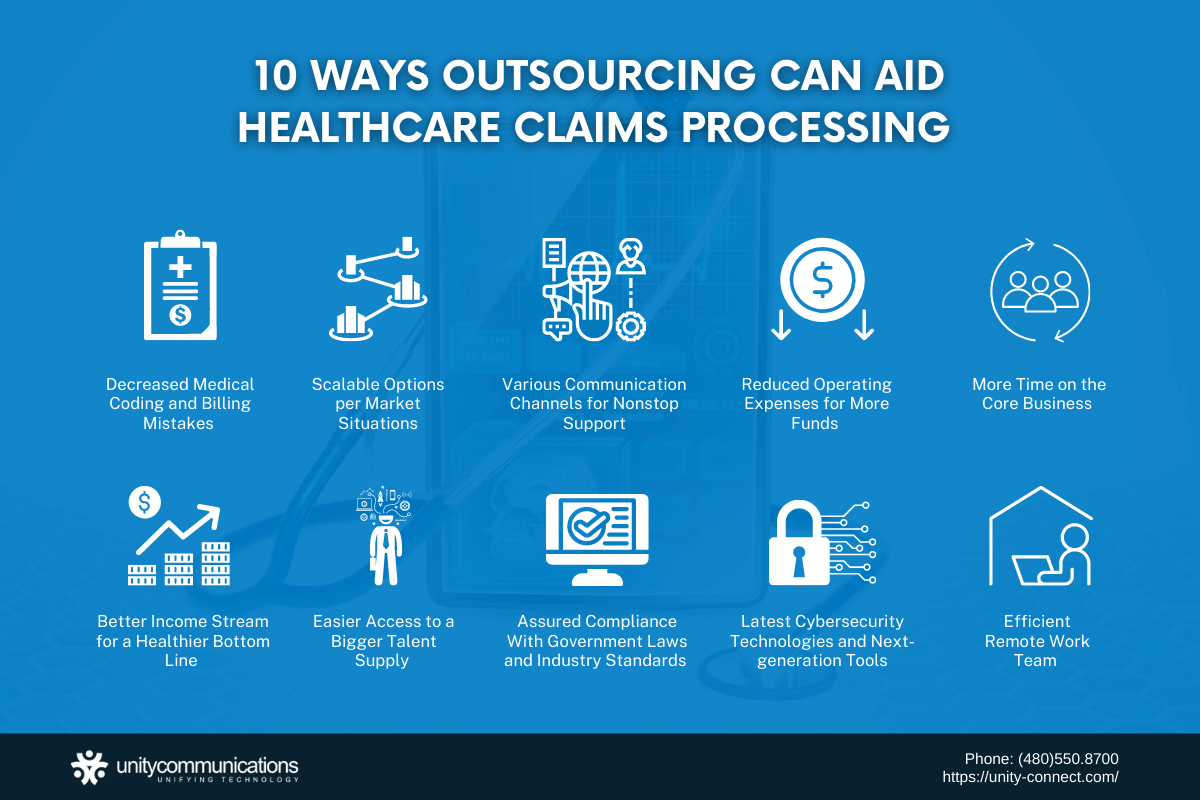
Consider these ten advantages of healthcare BPO services when outsourcing:
1. Decreased Medical Coding and Billing Mistakes
BPO providers have teams of knowledgeable medical coders and billers able to handle difficult and time-consuming insurance claims. These groups receive constant training to upgrade their skills and technical capabilities.
Outsourced contractors also process and send accurate and timely claims. They reduce insurance claim denials to expedite revenue collection for their clients.
Medical coding and billing errors and interruptions affect claims processing. Errors might result in:
- Poor employee morale. Lower-than-expected collection due to errors might mean a tighter budget, but employees’ working hours stay the same. This raises the chance of burnout and high turnover.
- Sluggish growth. Healthcare providers have difficulty expanding their facilities or services for better customer experience when cash flow concerns arise.
- Higher ongoing costs. Declined claims translate to more work and additional fees for claims resubmission.
Service providers specialize in medical coding and billing activities to help reduce errors that increase healthcare claims costs. They can decrease unclean claims, duplicate billing, authorization oversights, and inaccurate data encoding.
2. Scalable Options per Market Situations
A third-party vendor can scale up or down depending on an insurer’s business needs and operations.
Scalability provides insurers additional support when they are swamped with medical claims. A BPO provider supplies them with more teams and resources to address rising demands. They can also reduce the size of the third-party team when business transactions are slower.
3. Various Communication Channels for Nonstop Support
A BPO company uses different communication platforms to provide ongoing support services to insurers. Customers and patients can contact companies using their preferred method, including:
- Fixed-line or mobile phones
- Short messaging service
- Self-service portals
- Live chat
- Social media
Below are some advantages of having this omnichannel capability:
- Automates policyholder outreach by sending regular notifications of premium dates, new products and services, and company updates
- Retains customers longer due to increased accessibility
- Establishes a continuous and seamless interaction with customers regardless of the communication platform
- Delivers faster response time for more efficient healthcare claims processes.
4. Reduced Operating Expenses for More Funds
Businesses of all types outsource non-core functions to reduce costs and improve operational processes. In particular, delegating recruitment activities reduces employment advertising, hiring, onboarding, and training expenses.
Organizations also do not need to invest in new facilities, infrastructure, or equipment to outsource. They do not have to worry about maintaining digital and physical assets. Instead of setting up another in-house department, they can convert office rooms into more valuable spaces.
A BPO company deals with all these expenses on its client’s behalf. So an insurance provider has more capital for important ventures.
5. More Time on the Core Business
With the help of healthcare BPO services, management, and staff can spend less time on tedious tasks. Secondary activities are vital for any organization to stay profitable. But they take up valuable resources better used for more critical tasks.
Outsourcing costly tasks to a BPO partner gives insurers more time and energy for customer care and service. By making clients your top priority, you build loyalty and increase sales.
Higher revenue translates to:
- Bigger funds for insurance claims
- Larger budget to promote products and services for a broader market reach
- More diversified insurance services
- Quicker access to credit from financial institutions such as banks
- Improved staff compensation package
- Higher spending on employee training and technology
Outsourcing also enhances a company’s image and competitive edge. Focusing on its core competencies allows it to stay competitive in the long run.
6. Better Income Stream for a Healthier Bottom Line
A BPO provider efficiently collects payments and claims. It is an expert in pursuing and recovering long-overdue balances, unpaid receivables, and outstanding claims.
A service provider can help insurers monitor and retrieve unpaid amounts to increase collection. It works more effectively than an in-house team and performs collection activities ethically and legally.
Also, it reduces or eliminates mistakes in medical coding and billing by scrubbing or clearing claims to make them even more accurate. It then sends claims to third-party insurers for speedier approval and payment.
7. Easier Access to a Bigger Talent Supply
Healthcare organizations face staff shortages due to high turnover, stiff industry competition, and mass retirements. Adding to these are major events such as the pandemic lockdowns and the Great Resignation of 2021 when a large number of employees in the U.S. left work voluntarily.
Outsourcing addresses an insurance provider’s employment requirements. Service providers in the healthcare BPO industry operate in various locations worldwide. Such a setup gives them access to a large, global talent pool.
Check out the different types of outsourcing:
- Offshore. The BPO provider’s activities are stationed in a country far from the insurer’s physical office. For example, the healthcare organization is in Canada or the UK. The service provider is in Ukraine, India, or the Philippines, where plenty of skilled, English-speaking contractors are available.
- Nearshore. Service providers manage their outsourcing operations in a country near the insurer’s headquarters. For instance, the BPO partner is in Ukraine, while the insurer’s main office is in an adjacent country such as Hungary.
- Onshore. The operations of the third-party vendor and the insurance provider are in the same country. Their headquarters can be in different states. An example is a large-sized insurer hiring a BPO company in Arizona.
8. Assured Compliance With Government Laws and Industry Standards
Federal regulations and industry requirements govern the healthcare industry. They are changed, revised, and updated periodically to align with the interests of affected groups.
But such dynamism makes health claims and medical coding and billing more demanding. Below are some systems and laws that the insurance and healthcare sectors must comply with.
- The Health Insurance Portability and Accountability Act (HIPAA) is a guideline the federal government enacted in 1996 to safeguard patients’ sensitive health information from being disclosed without their prior knowledge. It also covers electronic medical records.
- International Classification of Diseases (ICD) is a set of medical codes healthcare providers use to file and process medical claims. Since 2003, ICD has been modified to match the World Health Organization (WHO) standards. ICD is part of HIPAA.
- Current Procedural Terminology (CPT) is a group of codes in numeric or alphanumeric characters designated to every healthcare service. Insurers use CPT to calculate the amount to pay policyholders and healthcare providers.
- Healthcare Common Procedure Coding System (HCPCS) is a coding system that Medicare uses for reimbursements. It details what medical supplies, products, and services insurance claimants can access. HCPCS is pronounced as “hick-picks.”
- A diagnosis-related group (DRG) is a medical system determining a patient’s hospitalization costs. Public insurers, Medicaid and Medicare, use DRG to compute the expenses for reimbursement to insured individuals.
Insurance providers can easily comply with federal policies and industry requirements when they hire medical BPO services. A service provider tracks the latest updates and trends to help insurers avoid violations that might lead to penalties and lawsuits.
9. Latest Cybersecurity Technologies and Next-generation Tools
Insurance providers invest in the latest healthcare claims management systems to maximize collection and limit losses. But cybersecurity networks are not their specialty and hence not their priority.
BPO providers use advanced cybersecurity solutions to protect their clients’ information technology (IT) infrastructure and websites. They can defend against unauthorized access and data breaches better. Their solutions are handled by IT specialists who regularly deal with data hacks, scams, thefts, breaches, and cyberattacks.
Additionally, service providers have the manpower and expertise to use these cybersecurity solutions to fully monitor and protect an insurer’s healthcare claims data and other sensitive information.
BPO companies also invest in the following technologies to offer insurance companies newer and better ways of doing business:
- Cloud computing enables all software, applications, and big data to be stored and managed virtually.
- Artificial intelligence (AI) is the simulation of human intelligence in machines. Integrating AI into the workflow boosts productivity at reasonable costs.
- Robotic process automation (RPA) lets a software robot perform certain processes, allowing employees to focus on more urgent and high-value tasks.
- The Internet of Things (IoT) refers to interconnected physical objects or devices that use the Internet to exchange data.
10. Efficient Remote Work Team
A BPO provider offering healthcare BPO services has proper management, clear-cut workflow protocols, and tight security measures for its remote work team. The following are ways it makes its WFH contractors productive and effective:
- Tight remote work policy. It instructs members on what to do and what not to do for better employee conduct. Setting ground rules from the start is important for smoother workflow, collaboration, and teamwork.
- Reliable collaboration tools. Its team depends on user-friendly communication applications (e.g., Zoom, Skype, Asana, Slack, or Microsoft Teams) for seamless and real-time communication.
- High-level security data. It uses virtual private networks (VPNs) and dependable antivirus software to encrypt and protect internet data from potential attacks. Multiple passwords for groups and individuals are also applied.
- Regular online meetings. A third-party team often holds videoconferences, meetings, or huddles to track work progress and each other’s well-being.
- Fully equipped remote staff. A BPO company provides WFH employees with the hardware and software tools needed to get the job done.
The Bottom Line
Outsourcing helps address the challenges in healthcare claims processing that insurance companies face amid the pandemic. In uncertain times, this business practice is a tried-and-true way for them to save money.
Outsourcing also offers insurers the best of both worlds. First, it reduces costs to free up more funds to pay claimants. Second, it delivers timely reimbursements and enhances the public image of insurance companies.
Being well-informed about outsourcing is essential. It increases insurers’ chances of achieving business goals for the benefit of their policyholders.



