IN THIS ARTICLE
Written by Joyce Ann Danieles
Contents
In-house workers for medical organizations are top contributors to a company’s continued success. These workers have the skills and capabilities required for efficient daily operations. But they sometimes cannot adapt to changing healthcare processes, such as medical bill review services.
Many organizations see business process outsourcing (BPO) as the go-to method for acquiring cost-effective, streamlined operations. In particular, healthcare BPO eases the tedious process of validating massive billing documents.
Let’s explore how this strategy affects your company’s growth and lets you focus on providing quality patient care.
Understanding Medical Bill Review Outsourcing

Hundreds of people visit healthcare organizations every day, for consultations and follow-ups, as a result of illness, accident, or routine check-ups.
As a result, in-house staff has a backlog of bills that need immediate processing and validation. Although the process sounds simple, it involves massive amounts of data and digits. A mistyped word or number can lead to complex issues.
Accurate and timely billing reduces loss and helps provide quality healthcare. Thus, back-office workers are under pressure to ensure zero miscalculations or errors. To avoid overworked employees, healthcare providers outsource their medical bill review services.
BPO companies expedite the medical bill review process at affordable costs. They use skilled employees and advanced technologies to perform repetitive tasks efficiently. They allow medical providers to prioritize high-quality patient care by offering the following healthcare BPO services:
- Validate hospital bills based on state-specific fee schedules and reasonable rates
- Pinpoint questionable charges, billing practices, and treatment options
- Identify discrepancies between documented services and billed charges
- Track hidden double payments resulting from complex billing practices
- Implement programs to help provide cost-efficient patient care
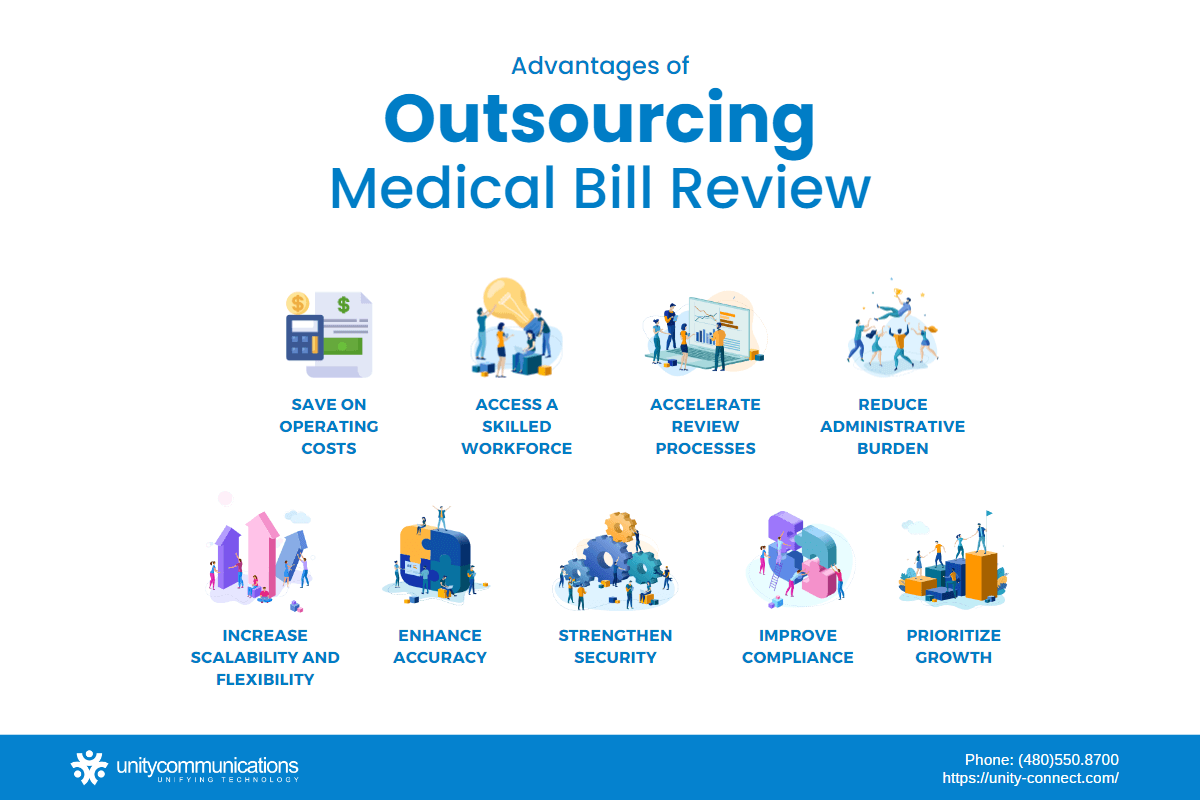
Nine Key Reasons Outsourcing Medical Bill Review Services Is Ideal
Inaccurate medical bills bring significant financial losses for healthcare providers, insurance companies, and patients. And they also can discourage patients from seeking care: According to a My Medical Score report, medical billing errors cost Americans more than $2 billion yearly. If appropriately captured, medical billing could fund more critical projects to boost healthcare services.
Medical institutions seek third-party support for their back-office functions to avoid wasting funds. BPO companies specialize in handling bill reviews. Healthcare businesses can thus focus on improving their core products and services without worry.
Superb patient care and error-free billing lead more people to trust and patronize health offerings. This advantage results in the healthcare organization’s expansion and success.
Read on to better understand why medical providers outsource their bill review processes.
1. Save on Operating Costs
Cost reduction is one of the healthcare BPO industry’s most crucial benefits. Organizations need considerable funding to hire and train skilled, full-time employees. They also need to invest in modern technology and comfortable office space. All these factors ensure bill review tasks run smoothly.
But by hiring BPO companies, medical providers no longer need to set aside separate funds for resources. Instead, they can enjoy review services through a long-term contract paid on a monthly billing cycle. They can also take a retail-type approach, paying for the service only after it is completed.
2. Access a Skilled Workforce
In-house departments employ talented healthcare professionals. But they lack time to train and upskill, which hinders their ability to adapt to rapid market trends.
Employees already deal with massive billing tasks as emergencies and hospitalizations increase. If backlogs overwhelm them, mistakes and miscalculations are inevitable despite multiple reviews.
Outsourcing medical bill review services provide access to skilled and well-trained employees. BPO service providers specialize in these processes. They must gain their clients’ trust to establish a good market reputation. So they execute the following measures to achieve that goal:
- Recruit, screen, and hire the best talent
- Offer competitive compensation package and benefits
- Host regular one-on-one coaching sessions and team meetings
- Train employees through workshops, seminars, and team-building activities
- Monitor, evaluate, and empower employees
- Provide flexible work arrangements and performance incentives for retention
When hiring medical BPO services, healthcare businesses no longer need to worry about setting up a full-time staff. They can hire medical bill review experts from third-party service providers at reasonable rates. Most importantly, they can immediately tap into these workers to scale their operations.
3. Accelerate Review Processes
Medical bill review services involve complicated datasets and processes. Employees confirm confidential and mathematical data to ensure cost efficiency for medical providers, insurance companies, and patients.
Urgency and accuracy make the medical bill review process difficult. Employees need to work fast to avoid prolonged payment delays. But they also need to prevent errors and miscalculations. Adding to that are the other tasks they must complete and the pressure they face during hectic seasons.
Medical providers thus rely on BPO companies to speed up their bill review processes. With modern solutions, skilled third-party employees handle such tasks with ease. Despite the fast-paced procedure, there is a low chance of mistakes because contractors focus only on validating medical bills.
4. Reduce Administrative Burden
People visit hospitals and clinics for both minor and important health concerns. As the number of patients surges, administrative tasks also increase. When stacks of medical bills hinder employees, the quality of patient care goes down.
Outsourcing medical bill review tasks help healthcare businesses reduce administrative work. Medical providers can entrust back-office activities to BPO companies specializing in the field.
Furthermore, advanced technology automates repetitive bill review services. It lets the BPO team complete assignments immediately. This capability allows employees to confidently provide healthcare products and services.
5. Increase Scalability and Flexibility
Medical providers and insurance companies might struggle to scale their medical bill review services due to labor, infrastructure, and office space expenses. In addition, they must guarantee uninterrupted operations as they grow—even during peak illness season.
Businesses must ensure their infrastructure purchases and team size fit their needs and budget allocations. Deploying new full-time employees is risky because they must undergo comprehensive training to guarantee smooth task completion. Picking a suitable workplace also demands significant funding and effort. Ample resources empower employees and encourage consistent and excellent performance.
Most healthcare providers contract with BPO companies to meet these demands. Third-party teams adjust their work strategies to match clients’ financial and operational needs. They align their enterprise and security policies with those of partners to avoid future problems.
With advanced solutions at their fingertips, skilled contractors provide immediate support to healthcare businesses. They assist their clients in ramping up their bill review tasks. Improved scalability and flexibility are clear advantages of healthcare BPO during slow or busy seasons.
6. Enhance Accuracy
Medical bill review services involve confidential information. Typos, miscalculations, and incorrect diagnostic codes happen when workers cannot keep up with abrupt changes in bill review processes. Inaccuracies due to overwhelming backlogs also result in the following issues:
- Denied insurance claims
- High operating expenses
- Slow revenue generation
- Frustrated and unsatisfied patients
- Poor healthcare quality
BPO vendors help healthcare businesses improve the accuracy of medical bills. They offer a cost-efficient approach to error-free bill review processes. Healthcare businesses must select the most reliable BPO partner to ensure success.
7. Strengthen Security
Since the pandemic, more companies have adopted advanced solutions such as artificial intelligence (AI) and cloud computing. The US federal government has mandated electronic health records (EHRs) since 2009 and rewards organizations that comply with incentives. But the ever-increasing quantity of electronic records are vulnerable to cyber threats.
According to the 2022 Protenus Breach Barometer, healthcare-related hacking incidents in 2021 reached a 44% year-over-year increase. The firm recorded 678 healthcare hacks in 2021, compared to 470 in 2020. It cited outdated security methods as the main reason for such cases.
Healthcare providers will suffer from the high cost of cyberattacks and mitigation efforts if they do not strengthen their defenses. They might lose their patients’ trust and loyalty. Bankruptcy and business closure are the worst-case scenarios resulting from such an event.
Sealing a deal with BPO providers helps strengthen information security. To maintain their reputation in the industry, BPO providers adhere to strict policies and procedures to protect medical data. They implement the following security measures to safeguard sensitive information:
- Multifactor authentication
- Data encryption
- Network and data monitoring
- Virtual private network
- AI-powered biometrics
- Antivirus scanning and mitigation
- Backup and recovery
8. Improve Compliance
Medical billing involves many tedious processes before the review phase. Employees must validate sensitive personal and billing data, from claim request registration to submission. During these stages, compliance with the data privacy requirements of the Health Insurance Portability and Accountability Act of 1996 (HIPAA) is necessary.
HIPAA ensures that organizations follow the general principles of using and disclosing protected health information (PHI). They must adhere to policies for oral and written communications. The law also mandates compliance with the security rule for electronic transactions.
BPO companies strictly observe HIPAA rules to maintain trust and a strong market position. They sign business associate agreements before handling PHI. They also conduct compliance analyses to ensure their in-house and client operations adhere to such rules and regulations.
9. Prioritize Growth
Review tasks are crucial to ensuring accuracy in medical bills. But they do not drive revenue. Spending considerable upfront capital on these functions does not guarantee returns. The activities also result in delays if their volume overwhelms primary projects.
Delegating medical bill review services to third-party companies allows medical providers to focus on enhancing their primary offerings. Healthcare businesses no longer need to worry about recruitment, technology acquisition, or leasing office space. Their BPO partners provide these resources and streamline bill review processes at affordable costs.
As a result, in-house teams have more time to work on their primary tasks. They can identify areas that require improvements. Freeing themselves from back-office tasks lets them develop innovative strategies to boost patient care. These capabilities help generate more savings and revenues in the long run.
Due to the listed benefits, many medical providers outsource their bill reviews and back-office processes. As demand increases, the BPO sector also continues to grow. Precedence Research thus expects the global healthcare outsourcing market to reach nearly $756 billion by 2030, registering a compound annual growth rate (CAGR) of almost 9.5%.
The Bottom Line

Reviewing medical bills requires considerable funding, time, and effort. Medical bill reviews are relevant for smooth payment processing. Still, they can hinder in-house teams from completing more important initiatives. Increased back-office backlogs also impede excellent healthcare service delivery.
Outsourcing such non-core tasks help reduce operating costs, ease administrative burdens, and strengthen security measures. Skilled workers and advanced technologies from BPO companies enable accelerated and accurate medical bill review services. These advantages allow healthcare businesses to prioritize product and service enhancement.
Expect to reap such benefits if you select the best service provider for medical bill processing and review. Reach out to Unity Communications if you want to boost patient experience at lower costs. The award-winning BPO company uses advanced healthcare solutions to streamline time-consuming administrative tasks, allowing you to prioritize your medical practice.





